Five signs you should consider surgery for acid reflux
By Margaret Riccardi, DO, Penn State Health
If you’re among the one-in-five adults in the U.S. who have gastroesophageal reflux disease (GERD), you know how uncomfortable the symptoms can be. More common in women than men, chronic acid reflux can cause painful heartburn, regurgitation, a constant bitter taste in the mouth, and even difficulties swallowing. Left untreated or unmanaged, it can progress to more serious conditions.
The first line of treatment for GERD may include over-the-counter antacids as needed and lifestyle changes, such as not lying down for at least two hours after eating, losing weight, and wearing nonrestrictive clothing. Doctors may also recommend eating smaller meals and limiting trigger foods, like fried, fatty or spicy foods and caffeinated or carbonated beverages. If those efforts don’t work, your doctor may prescribe medications that reduce or stop acid production.
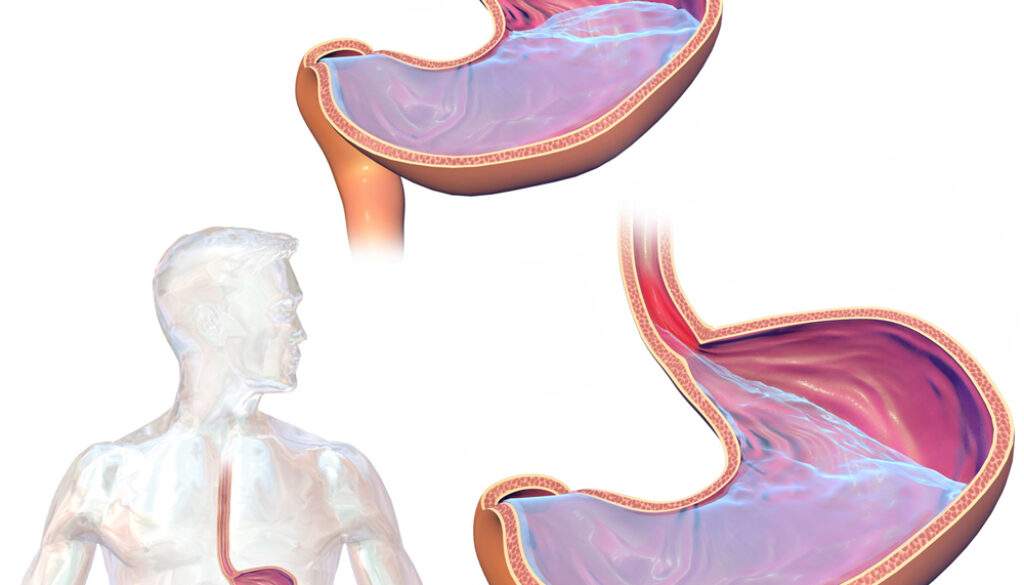
GERD is caused by a defective barrier between the stomach and the esophagus, due to a hernia or from having a weak valve, that allows stomach contents to move up into the esophagus. To treat the underlying cause, your doctor may recommend minimally invasive surgery.
Here are five signs that it might be time to consider surgery for your GERD:
1. Your medications don’t control your symptoms.
If lifestyle changes and over-the-counter antacids don’t alleviate your acid reflux, your doctor may a prescribe proton pump inhibitor (PPI) or similar medications to reduce or stop acid production. But 38% of people taking PPIs for GERD don’t get complete relief from their symptoms. These patients may be good candidates for surgery.
2. Your medications work, but you want to stop taking them.
Some patients find effective relief for their GERD symptoms with PPIs. But these medications can cause side effects including nausea and vomiting, diarrhea, or rash. Surgery can treat the underlying cause of GERD, eliminating the need to take PPIs.
3. You’re experiencing different or worrisome symptoms.
Sometimes GERD can be silent in the sense that it doesn’t present the typical reflux symptoms of heartburn and regurgitation. Instead, it may cause a cough or hoarseness, as the reflux goes all the way up to the vocal cords. You also might feel as if there’s something stuck in your throat. Chronic throat clearing can be tell-tale warning sign that you have GERD. In older patients especially, GERD can contribute to chronic aspiration, where regurgitated food and liquid enter the windpipe, or recurrent pneumonia.
4. You’re concerned about developing serious complications from GERD.
Overtime, GERD can cause esophagitis, an inflammation of the esophageal tissue. This often painful condition can make swallowing difficult. Another potential complication that can also interfere with swallowing is an esophageal stricture, or narrowing of the esophagus caused by scar tissue from acidic reflux. And finally, about 10 to 15% of patients with long-term GERD will develop Barrett’s esophagus, an abnormal change to cells lining the lower part of the esophagus, which may become precancerous.
5. Your doctor has recommended surgery.
If you’ve had to take medications for GERD for a long time, have uncontrolled symptoms or are experiencing complications from the disease, your doctor may recommend a surgical solution.
What to expect with minimally invasive GERD surgery
Your surgeon will use a minimally invasive approach to treat your GERD, making small incisions to recreate the valve between the stomach and the esophagus. This may involve inserting what’s called a LINX device, a ring of tiny magnetic beads that wraps around the junction of the stomach and esophagus. If a hernia is present, that will be repaired, too. The surgery typically takes about one-and-a half hours, and patients can go home the same day. In cases involving large or complicated hernias, the surgery can take a bit longer, with patients usually staying in the hospital for one night and restricted to a liquid-only diet for a few days afterward.
To learn what specific, minimally invasive approach is recommended to treat your GERD, your doctor will order or review tests to see the extent of the reflux and related complications and to see if other diseases or conditions may be contributing to symptoms.
Dr. Margaret Riccardi performs minimally invasive surgery at Penn State Health St. Joseph Medical Center in Reading, PA, to treat common and complex diseases of the foregut — the area comprising the esophagus, stomach and small intestine. Want to discuss further? Stop by the Penn State Health booth at 2023’s Guts & Glory Digestive & Wellness Expo to talk with Dr. Riccardi or call 610-378-7900 to schedule an appointment.